Register for online access to your GP electronic health records and understanding
Well done. You are a couple of steps away from getting access and understanding of your GP electronic health records. Watch this short video which tells you what to do next.
Register your PIN NUMBERS
You will need to collect this from the receptionist or ask for it to be emailed to you. You will need to speak to the receptionist who can then arrange this for you.
See videos which show how to download and register your pin numbers on Evergreen Life PHR and Patient Access
For the best experience from the practice, we recommend you use Evergreen Life PHR.
You may also wish to use Patient Access and / or the NHS App if you wish to use an app to access your childrens or another patient you care for and have permission to access their records too.
Learn more about Records Access and Understanding here
Do you know how many other patients have got access to their GP electronic health records at Haughton Thornley Medical Centres?
| Patients with the Problem / Medication | Total number of patients | Percentage with access |
| Number of patients with access to their GP electronic health records | 10414/127625 | 81% |
| Patients with Prediabetes | 871/1058 | 82% |
| Patients with Diabetes (Type 1 and Type 2) | 814/973 | 83% |
| Patients with Type 1 Diabetes | 71/74 | 95% |
| Patients with Ischaemic Heart Disease | 363/460 | 78% |
| Patients with Heart Failure | 100/124 | 80% |
| Patients with Atrial Fibrillation | 187/242 | 77% |
| Patients with Obesity | 579/611 | 94% |
| Patients with Rheumatoid Arthritis | 67/77 | 87% |
| Patients with Asthma | 1692/1936 | 87% |
| Patients with Low Back Pain | 3158/3659 | 86% |
| Patients with Chronic Obstructive Pulmonary Disease | 297/391 | 75% |
| Patients with Depression / Anxiety with Depression | 3505/4048 | 86% |
| Patients with Attention Deficit Hyperactivity Disorder | 73/86 | 84% |
| Patients with Cancer confirmed | 361/448 | 80% |
| Patients with Is a Carer | 393/438 | 89% |
| Patients with Deep Venous Thrombosis | 125/159 | 78% |
| Patients with Pulmonary Embolus | 80/95 | 84% |
| Patients with Chronic Kidney Disease | 290/398 | 72% |
| Patients with anti-coagulation therapy ie warfarin, sinthrone | 27/33 | 81% |
| Patients with Thyroxine | 468/548 | 85% |
| Patients with Methotrexate | 27/29 | 93% |
| Patients who were Pregnant from 10 months ago | 66/67 | 98% |
| Patients on Learning Disability register | 61/84 | 72% |
| Patients who have ever had a URTI or viral infection | 6278/7273 | 86% |
| Bengali patients with access to their records | 1428/1627 | 87% |
| Patients on gold standards palliative care framework | 108/157 | 68% |
| Current patients who have ever Ordered Prescriptions Online | 4002/12725 | 31% |
| Patients at Haughton Vale Surgery | 4220/5554 | 75% |
| Patients at Thornley House Medical Centre | 6175/7147 | 86% |

Currently we have 2895 patients who have tested positive for covid19 since the start of the pandemic, and of those, 2666 (92%) have full records access and understanding
How are we doing with enabling patients to access their GP electronic health record?
We have enabled patients to access their GP electronic health record since 2004 and now have over 10,000 patients who have requested access to their records on-line. Many more patients are also ordering repeat prescriptions on-line and cancelling appointments on-line (which gives somebody else the opportunity to take that appontment instead easily)!
In an attempt to try to understand better the needs of patients who have access to their GP electronic health record, we created a local “EMIS code” such that the system clearly states that this patient has access to their records. We have called it “Patient Access to E-Health Record” or “Patient Remote Record Access Enabled”. This should be in the Active or Significant Problems in date order list on the Summary Page when patients first log on to see their records (you may well have to scroll down the page to see it). You can see an example of what it looks like by looking at the Test Patient’s Record too.
Why code the fact that the patient has access to their electronic health record?
All patients get the same standard of care from the practice whether they have access to their records or not. However there are some specific advantages to patients who have this code added:
- We know that you have access and so may ask you questions about if and how having access has helped you in any way when away from the practice
- Clinicians may be more inclined to write in your records advice which may help you to manage your condition better eg websites that they may want you to look at to support your care or treatment
- Clinicians may write further details about why we have chosen a particular course of action which makes more sense to you. For example we may see a test result and advise you to start certain medication. There may be a further explanatory note which explains why that medication has been started. Of course if it is necessary then we would ALWAYS contact you by phone or letter and not assume that you will pick up a message that is in your record.
- It is hoped that patients with this code would also be invited to access other electronic health records once they are also made available for you to see. That is why the code says e-health and not just the GP record.
- Presently we have over 10,000 patients who have this code.
- Occasionally patients may lose the right to access their electronic health records for instance if they suffer a catastrophic mental health problem and it is deemed unsafe for the patient to access their records. This would be done in the patient’s best interests. An easy way of knowing if the access has been revoked would be to see if the code is still active or whether it has been removed.
So how are we doing ?
We are pleased to report that we have over 10,000 patients with the code confirming they are able to access their records with no significant problems to date. The numbers of patients are going up weekly as more and more questionnaires are filled out and handed back. Every age band now has at least one patient who has access indicating that Records Access is for everybody. You might know somebody who does. Why don’t you ask them to get in touch with the practice to find out more, click on the link below for them to print off or ideally ask them to e-mail us on [email protected] to find out more.
What else can you do to help?
If you have enjoyed access to your electronic health records then why don’t you ask the rest of your family, friends, colleagues and work friends to get access too. You never know, it could help them one day too.
Ask them to complete an online questionnaire now. They will need to collect their pin numbers from the receptionist too.
What about patients who do not know how to use the internet? Is there any help for them?
There are courses available in the local library and people in the community centres locally who can show them how to go on-line, access their records and learn more about their own health. Members of our Patient Participation Group and our staff would also be happy to help.
What do we want patients to do with Records Access?
Hard to say really because you are individual and you will know why you want access to your records. We know that patients access their records have a better understanding of their own health and are “ahead of the game”.They know what is in their records and find it easy to see any recent letters, test results or scan results and what was discussed in previous consultations.
We would like you to understand your condition better so that you can make better choices about your health and that of your loved ones. Remember your doctor or nurse can also help you with what choices you can make to improve your health. Monitoring your own health and storing aspects eg weight, blood pressure or smoking status can help too. You can find a variety of other trusted sources on the practice website – via the Patient Control Panel including NHS Choices, Clinical Knowledge Summaries and Common Problems You Can Solve. Watch this video to help you to understand blood test results and Lab Tests Online.
Guardian Article: Patients need access and understanding of their electronic health records
About Records Access
| Haughton Thornley Medical Centres allow you to view your electronic health record via computer, laptop, smartphone or tablet. You first need to register and consent to use the system in the GP practice. What is the Online EHR Viewing System? The system allows you to easily and quickly view the electronic medical information held about you by your GP Practice.The information is presented to you in a format that is easy to navigate and offers you links to resources such as patient information leaflets about diseases, tests, investigations, support groups and medications etc. Registering and consenting to use the EHR Viewing system To be able to use the system you must be able to access the internet via a PC, Tablet or Smartphone.You have to collect your PIN NUMBERS from the receptionist or have them emailed to you so that you can REGISTER on-line. You also need to complete an ONLINE QUESTIONNAIRE. We will then process your request and then contact you to confirm your access and complete the consent process.Any data held by the practice concerning you is subject to the regulations laid down in the Data Protection Act (1998). The consent is between you and your GP Practice. What can I see on the Online EHR viewing system? The system allows you to view the following areas of your medical record: A summary that gives you the most important and recent entries in your health record. Consultations including: date, practitioner seen, reason for visit, history, examination, outcome, investigations, etc. Medical Record showing diagnoses, investigations, and procedures Allergies. Patient Information Leaflets linked from the diagnoses in the medical record section.Results showing all investigations such as blood results, liver tests, blood pressure etc. Vaccinations. Medications. Letters to and from the GP. The system also allows you to send messages to the practice Why have an Online EHR viewing system? There are many reasons to provide you with access to your medical information. A few of them are listed below: ‘We want to develop a culture of openness, honesty and trust; to ensure that patients have the information they need to make informed choices; and to enable patients to become equal partners with health care professionals in making decisions about treatment and care.’ This is the response to the Department of Health from the enquiry into the Bristol Royal Infirmary Enquiry. ‘Patients have the right to see their medical records, though in practice much communication between professionals is not available to the patient concerned. Patients often do not know why they are being referred, or what is being said about them’ The NHS Plan Haughton Thornley Medical Centres believe that it is important for improved patient care and education that you are involved in your healthcare as much as possible. Advantages to you, the patient: No queuing to get results You can check the accuracy of your medical record You are empowered to become more involved in your own medical care REMEMBER – To protect your privacy, as with all password protected applications on the internet, logout of the system when you are finished. |
Background on Record Access
Following the introduction of Patient Record Access by Dr Amir Hannan in 2004, Haughton Thornley Medical Centres patients have pioneered internet access to their full GP electronic held record. This means that patients who are registered to use the service can access their health records anywhere and any time that they have internet access. The Practice has since gone on to recruit over 10,000 patients for this purpose.
Initially, Dr Hannan held meetings once a week at the Practice where patients wanting to access their medical records were invited to a presentation on what Records Access entails, what the possible benefits are, a summary of some of the issues and locally how we are trying to overcome them.
One important aspect of the introduction of Record Access was the local Care Record Development Board which advised clinicians, patients and the local health and social care organisations on aspects of “records access”. One of our Haughton Thornley patients, Yvonne Bennett, then also began to give presentations on “Records Access” from a patient’s perspective.
Up to 20 patients attended each of the meetings where there was an opportunity to raise questions. Following each meeting, patients were invited to sign up for records access after giving due consideration. This approach was generally well received and helped us all to gain confidence in the process. Most importantly it helped Dr Hannan and the other partners at the Practice to identify the main issues and also how they could best be resolved.
One challenge the Practice faced was trying to accommodate the number of patients who wished to attend the introductory meeting and for Dr Hannan himself to be sufficiently available to present to an ever growing number of patients who wished to access their records. In an attempt to try to stream-line the process and enable patients to access the information at a time of their choosing and in the comfort of their own home, Dr Hannan produced a DVD. Patients were then invited to take the DVD home to watch the different chapters on their TV sets. Following this, they were asked to complete a short questionnaire which ensured that they had considered the issues and felt comfortable with going ahead and signing up for the Record Access service.
The videos that were produced are now available from the internet (see links below) and are hosted on You Tube for our patients and anyone interested in Record Access to watch at any time. Each video lasts up to 6 minutes.
After you have watched the videos and read the other material on this website, you may be in a position to complete the questionnaire. The partners experience so far is that most people are eligible for accessing their medical records so long as you understand the issues and are willing to accept the potential risks as well as the benefits.
Note to individuals who are not patients of Haughton Thornley Medical Centres
If your practice does not offer full records access and you are based in the UK then please ask your GP to get in touch with Dr Hannan if you feel they would be interested in understanding more about our experiences here at Haughton Thornley Medica Centres.
You Tube videos explaining the benefits and issues with Records Access and Undertanding
| Video | Description |
| Introduction | An introduction from Dr Amir Hannan to Records Access and additional video content available from this site |
| Blood Pressure (BP) & Weight | A reminder that Records Access is not just about checking your records, but also an opportunity for you to keep your health record as up to date as possible by checking your Blood Pressure (BP) and weight and informing your doctor what the details are at your next visit |
| What do we want you to do? | How to go about accessing your health record and what to expect when you do |
| The benefits | Describes the benefits of Records Access and why we believe you should consider registering to use this service |
| Some issues (part 1) | Password protection, increased demand on a stretched service. Mental Health, challenges for non-English speaking patients |
| Some issues (part 2) | Significant events e.g. termination of pregnancy |
| Some issues (part 3) | Consultants may not be aware that you are accessing your health records online. You may now see letters before your GP does |
| The BIG issues (part 1) | News that you don’t understand |
| The BIG issues (part 2) | Handling unexpected news e.g. a shadow on the lung on a chest X Ray |
| The BIG issues (part 3) | Wrong letter in notes and children and Record Access rights |
| The BIG issues (part 4) | Dealing with third party information and special consideratio eg child protection and psychiatric notes |
| Patient – the advantages | A patient’s perspective on the advantages |
| Patient – What You See Is What You Get (WYSIWYG) | What else could WYSIWYG mean? |
| Patient – Frequently Asked Questions (FAQ) | A range of questions that have already been asked by patients |
| Local Care Record Development Board | What is the local Care Record Development Board and how does it help to protect patients and clinicians |
| How can you help? | What can patients do to help the system and clinicians |
| Next steps | What are the next steps that you should take to get access to your health records? |
Top 10 reasons for having access to your records and understanding
- 1 It can make managing your health easier
- We give you all the tools you need to understand your health better by linking some of the best heath information websites with your own GP-held electronic health record. We bring your personal HealthSpace in the same place so that you can even access your personal data that you may be monitoring eg blood pressure, peak flows, blood sugars, smoking or weight.
- 2 It is completely FREE
- There are no long-term commitments or hidden charges when you use Records Acccess. The service is completely FREE as part of the NHS care that you get – free at the point of delivery for all.
- 3 It is intuitive
- We’ve brought together all the information you need to enable you to decide if you want access to your electronic health record as easy as possible. We have even moved a paper based questionnaire to an electronic one so that the only paper you have to print is the consent form and we’re even working on an electronic form for that too! There is no software to install, and no complicated manual to try to understand. The practice web-site has everything you need to start looking at your electronic health record and make sense of what it means and what you could do next!
- 4 Record Access is powerful
- You can easily see your records, medications, past medications you have been on, immunizations you have had, blood tests, X-Rays, CT scans, MRI scans, ultrasounds, letters from any hospitals or other clinics or services you may have visited and from there relevant links to websites that give you more information about health conditions you suffer from or may be at risk of developing.
- 5 There are few limits
- Although we have started you off by showing you trusted websites that we vouch for, you can even store your own personal favourites that you have come across in HealthSpace as well as issues you may have that you wish to discuss with another health care professional when you next meet them. Best of all, these can be used in any setting that has internet access – in the surgery, when you go to the hospital, when you have a medication review with the pharmacist, on your iPhone or other internet enabled gadget or when you are on holiday, 1000s of miles away from home!
- 6 It is secure
- We employ multiple layers of security to make sure that your account and your data remains private and secure. Nobody can access your record without your permission. The software developers are constantly refining the process and ensuring it meets the highest standards of security so that you know your data is safe and secure
- 7 Record Access is proven and growing
- Over 80% of GP practices have now been enabled to allow their patients to access their GP electronic heath records just like ours.
- 8 We are small enough to care
- We have a small team in the practice that deal with any queries relating to Records Access. Katie Rumney based at Thornley House Medical Centre is the main contact although Dr Hannan is very happy to call you for further assistance too. We are able to respond to queries quickly and easily and post any general issues on the practice website under FAQs.
- 9 We are governed
- We pledge to respect your privacy but also your right to access health information whenever you need it and wherever you need it (subject to certain pre-conditions as set out in the Data Protection Act). Any data that you collect is kept completely and absolutely confidential. To date, we have developed the website on goodwill and altruism and are keen to keep advertising out. We have shared our views with many people inside the NHS and outside it too sharing our experiences with all
- 10 We are listening
- Have a feature request? A suggestion? A complaint? We are always open to new ideas, and we always welcome constructive criticism. The best ideas come from you. Why don’t you send any comments to [email protected], ring the surgery and leave a message for us or come along and voice your opinion at the next Patient Participation Group meeting.
- Because you or your loved one may never know when, where or why you may need healthcare and access to your electronic health record
What are the benefits and challenges associated with patients accessing their GP held Health Record?
Benefits
- GP/Healthcare
The patient has an active role in their own healthcare and develops a good relationship with their GP and Practice. This is being backed up with the ‘Choose-and-book’ option where the patient can choose which hospital they would like to be referred. - Repeat Prescriptions
These can be ordered via the internet whether you take advantage of the access to records or not. You must also register for this service. - Results
With access to your medical records you can check any results or letters - Holidays
You may be in another country and taken ill. You may decide to allow the doctor access to your records (a personal decision). It might be that you forgot to order your repeat prescription and need it to be ready on your return. You can do this by using an internet café. You usually find such facilities in most holiday destinations. This has been tried very successfully from abroad. - Appointments
Appointments at the Practice can be viewed on screen and cancelled if you wish. If you are going to see a healthcare professional outside your area you can allow them to see your records online (if facilities exist) or print out the relevant information and take it with you. (The date will be on the bottom of the printout) - Community
It might be that you are receiving care at home and it is necessary for latest results of tests to be known before treatment is given. You can check the results yourself or allow anyone else you see fit to do so. - Nursing Homes
If a relative is in a nursing home, and you have been given access to their records, by monitoring the ‘consultation’ section you can monitor their care. Records of visits by doctors along with comments by the doctor will be recorded here. This could be done from anywhere in the world. - Relatives
Should you wish, you can share all your health records with relatives or just part by printing the part you wish to share. - Time
For most people there is never enough time — doctors included. Much time can be saved by ordering repeats via the net. You can track the details and progress of your request before instructing the chemist to collect. Blood results, x-rays or letters can be checked. If they are normal it saves you time not having to travel to the surgery (can be lengthy & expensive if you don’t have your own transport). It also leaves a free appointment allowing the doctor to see someone who is in need of an appointment. - Information
You can easily check information about any medication prescribed by clicking on the blue ‘i’ button listed next to your medication in the list. This also includes information on how to take the medication such as ‘on an empty stomach’ or ‘with food’ etc which is not always available when you receive tablets in bottles. You can check what results mean or check a condition and some help guidelines. There are links to support groups e.g. Diabetes UK . - Security
The system uses a similar security approach as online / internet banking IF you keep your passwords secure. Just as in the same way that you wouldn’t leave your bankers card and pin numbers lying around (particularly at work) and then wonder how someone managed to withdraw money from your account, it is essential that you do not leave your passwords where they can be found. This may also include at home if you don’t want family members to view your records. Don’t use obvious passwords such as names, birthdays or anniversaries etc.
Challenges
- Forgotten History
There may be something in your history you don’t want any family members to see. It might be information you had put to the back of your mind and are now confronted with it! - Bad News
You may read some bad news before the doctor has seen it. - Abnormal Results
Results may be abnormal and cause you to worry - X-rays
A chest x-ray may show a shadow and ? Cancer - X-rays
A chest x-ray may show a shadow and ? Cancer - What should you do! – The alternatives are the same for all three.
Ring the surgery and ask for a telephone consultation
If out of hours, don’t look at the results if you are prone to worry – wait until the surgery opens before checking
Speak with NHS Direct – 111 (available 24 hours)
Ring Surgery for out of hours number
Ring A&E only if you are feeling really unwell
Remember had you not had access you would not have known the results until either the doctor / Practice contacted you or you rang for the results - 3rd party information
You might want to tell the doctor something about your spouse/partner/child etc in confidence. If the doctor records the information and the patient then sees this it could cause problems. If the doctor doesn’t vital information may get lost or forgotten
The information may be malicious and again cause problems - Children
When is a child not a child?
Some children may be 12 years old but appear to be much more mature whilst others could be 18 years old but are still relatively immature
At what age should children have their own passwords?
What about a teenage girl who wants contraception but doesn’t want her parents to know?
Example Test Patient
There are 2 ways to view electronic health records with the test patient record. You can either use Evergreen Life PHR or Patient Access for FREE.
| User ID: | Email address: [email protected] Password: Haughton1 Memorable word: Thornley1 |
Keeping Your Information Safe
Guidance on privacy, confidentiality, security and consent
When our patients register for on-line services, some of the questions we are asked relate to the concerns over the privacy and confidentiality of personal health information and will that be affected once individuals have opened up to using the internet to access their personal information and request services.
In conjunction with Glen Griffith and advice from members of our PPG, we have put together this guide which we trust will help to give our patients an insight into this sometimes complex area and which we hope clearly demonstrates the many careful steps that have been taken to ensure that ‘patient information privacy’ and confidentiality remains the utmost priority for the services we provide direct to our patients.
As ever, we welcome your views and any questions you might have which can be raised in person or email [email protected]. Responses to such questions (no personal details will be included) might be used as part of our frequently asked questions page to help others.
Protecting your health information in general – some definitions
Privacy, is the right expressed by an individual to prevent access by others to themselves. For citizens enrolled with the National Health Service in the UK (NHS), it is only in exceptional circumstances (often when an individual requires protection eg on a witness protection programme) that individuals are able to retain total privacy. In those situations, ‘demographic data’ – name and address details – are prevented from being shared between agencies within the NHS. For the vast majority of patients however, basic information about them is shared fairly routinely but under strict confidentiality guidelines overseen by a Caldicott Guardian who is a senior person responsible for “protecting the confidentiality of patient and service-user information and enabling appropriate information-sharing” – safeguarding the interests of individual patients. An individual’s medical record is also subject to these strict controls on who can and can’t see medical information and on what grounds and this is how confidentiality is maintiained. The NHS has a published standard called the Care Record Service guarantee that makes this clear.
Further definitions on privacy and confidentiality and how it affects our patients can be found here.
Patient access to electronic health records – the steps taken to protect your privacy
Patients at Haughton Thornley Medical Centres have several options they can opt for to access services over the internet.
1. Ordering repeat prescriptions
2. Accessing their GP electronic health records
The first service can be accessed by patients by asking for their PIN (Personal Identification Number) from the receptionist and then registering on-line once they get home using those PIN numbers and as part of the process patients create their own unique passwords. Requesting the PIN number activates the patients account, without this, it is impossible for anyone to access the system – the system is therefore inherently secure and requires a positive action on the part of the patient to open it up.
Access to the full GP electronic health record requires a patient to also complete an on-line questionnaire. The questionnaire can be sent to patients via email (this ensures that we have the correct email details) once a request for access has been made – if a staff member takes your email details from you then you are already authenticated (i.e. we know you as a patient on our list).
Please note: It is possible to just sign up for ordering repeat prescritions and booking appointments on-line without having full access to the GP electronic health record.
What does all this mean?
By using this process, patients give the Practice their explicit consent to open up their records for internet access. No one other than the patient is able to access the record as unique PINs are issued in each individual case – patients (sometimes referred to as service users) are then able to complete the registration and change passwords to something more memorable and there is also a change password facility built in so patients may change a password from time to time. You the patient are then in control and you have the choice to share those PINs and passwords with whom YOU like. So, if you want your spouse and / or your children to access your records on your behalf then you are free to do so but the responsibility of sharing those PINs and passwords is yours.
Important note: If at any time you change your mind and decide you do not want others to access your GP electronic health record, you can change the passwords directly on the system. We can also switch off access to the GP electronic health record at any time if you so wish.
Please note: we do NOT recommend that you share your pin numbers or passwords with healthcare workers.
If somebody needs to know the contents of your electronic health record and you agree that they can see it then you should enter the PIN and password privately (like you would when typing in your PIN for your credit card) and then turn the screen to share it with the healthcare professional so that they can see your record. We also recommend that you log out of the system when the healthcare professional has finished. That way there can be no accusation that the healthcare professional has accessed your medical records without your authority.
One further consideration is what happens if you become unconscious and hence nobody is able to access your medical records because you are unable to give them permission. We recommend that everybody should have a contact name in their mobile phone called “ICE” which stands for In Case of Emergency. Paramedics, police, doctors etc. are trained to look in the phone of someone who is unconscious for this contact name and to then ring it. You may choose for that person whom you have nominated as your “next of kin” to have the PIN and passwords for this eventuality. They may then be able to pass the details on to the relevant body if they feel it is in your best interests. If you choose to do this then it may also be prudent to change your passwords at your earliest convenience too. This safeguards your privacy and of course protects the emergency worker from any accusation of inappropriate access to your record. This is something patients at Haughton Thornley Medical Centres thought of and again is an option for you to consider for you and your loved ones. By the way, having an “ICE” entry in your mobile phone makes sense whether or not you share your PIN and passwords details.
Once a patient has requested and been granted access to online services, there are a series of measures in place within the computer system to protect our patients information privacy and there are also a number of precautions that patients should be aware of themselves which involve good practice when accessing personal information.
The information security measures in place safeguard our patients from unauthorised access by any other individual and can be explained as follows:
- Accessing your GP electronic health record
- Using a memorable password as described here
- Do not leave your password in “secret” places that you think nobody will think of eg under your keyboard, in the drawer next to your computer etc etc.
- Get into the habit of changing your passwords regularly
And finally if you are still unsure about whether Records Access is for you then consider this:
What is more important for YOU – your LIFE or your REPUTATION. If it is your life and if you want the best possible care when you fall ill then you should probably consider GETTING ACCESS to your health record – it may save your life one day. If on the other hand YOUR REPUTATION is more important and you really do not want some “secretive information in your electronic health record becoming available accidentally or otherwise” then you probably ought to choose not to have access to your electronic GP record. Of course you can ALWAYS come and discuss this with your clinician, friends and family or whom YOU TRUST to help you make this decision. And of course do keep listening around you, on TV and the radio and in newsapers because this is a discussion and debate that no doubt will continue for a long time yet to come.
We at Haughton Thornley Medical Centres – in conjunction with Glen Griffiths and the Patient Participatin Group – are keen to support patients and the public to help understand some of the complex issues discussed here but also to offer assistance to get the best healthcare possible in a world where information is increasingly available 24 hours a day 7 days a week 365 days a year from anywhere in the world and available at the end of a click! We are keen to build a Partnership of Trust and this page has been produced to help support you, us and the system as a whole.
Please feel free to contact us on [email protected] if you have any further views, comments etc
Maintaining Confidentiality
Creating a safe password that is difficult for others to guess
Passwords are very important when accessing personal information over the internet (from your bank, supermarket or General Practice) because systems on the web are built to discriminate very carefully when incorrect passwords are entered. The system that we use at Haughton Thornley Medical Centres is case sensitive which means that not only are the correct order of letters,numbers and other characters required but it is also essential also to use the correct upper and lower case letters – THIS IS IMPORTANT TO REMEMBER WHEN CREATING YOUR PASSWORD!
We have assembled tips from some of our patients on creating strong passwords below.
- Include both uppercase and lowercase letters and at least one number
- Do not use birthdays
- Do not include your login name, a.k.a. username, in any form (i.e. as is, reversed, capitalized, doubled) or any other name
- Avoid words that can be found in a dictionary (including foreign and technical dictionaries) these include names.
- Do not use a password that has already been given as an example of a good password.
- Create an easy to remember password: One possible way to choose a good password is to make up your own acronym (an Acronym is something like NHS, TUC, GMPTE etc.,. Create a phrase that has meaning to you and pick the first letter of each word. Remember: a combination of numbers and letters is harder to guess or crack with a computer program.
For example:
- I love to shop for sandals in the Spring.” (Il2s4sitS)
- 12 x 12 are 144 (12x12r144)
- “I’m going to work out 3 times a week.” (Ig2wo3taw)
- “Last summer I caught a 30 inch striped bass.” (LsIca30isb)
- My password needs to be 8 letters long (mpntb8ll)
A similar method is to take out all the vowels from a short phrase.
For example:
“I work 8 hours a day.” (wrk8hrsdy)
Overall it is important that a password is something that you can easily remember now and in the future and that you ensure that loved ones are aware of your PIN and password if you feel you would like them to be aware of it in case of an emergency where you may yourself be unconscious.
Frequently asked Questions (FAQ)
Where is my confidential medical information held whilst I am viewing my online EHR and who has access to it?
The information you view on the online system comes from the clinical system in your GP practice. Portions of this information are encrypted (this means it is very difficult for someone else to intercept and read the information) and securely sent from the GP system to your PC web browser.
None of the medical information that is shown on the online system is held permanently on any computer except the computer which holds the original data in the GP practice.
When you log off from the online system or if a problem occurs with your computer, for instance a power failure, all your confidential medical information is cleared from the system.
Using the online system does not allow any extra people to view your medical information other than the people who would normally have access to it in the GP practice.
How will other people be prohibited from seeing my record?
To view your online EHR you have to identify yourself with passwords and PINs that only you know. Unless you reveal this information to someone else you will be the only person able to access your medical record via the online system
What if I find an error in my medical record or if I see someone else’s medical information?
If you find any errors or missing information in your medical record you can use the messaging system (if your practice has enabled it) to send the practice a message or alternatively you can tell the receptionist or discuss it with your GP. If you see someone else’s medical information you should immediately exit from the system and inform the practice staff.
What if I don’t want to register to use the PAERS System?
If you do not want to register to use the PAERS System you can still use all the practices’ services exactly as before. Your decision not to register will not affect your treatment or your relationship with your GP practice in any way.
What should I know about with regard to passwords I might use?
Passwords are all Case sensitive
Please remember there is a difference between O (letter O) and 0 (zero)
If you leave passwords lying around then the system is not secure
Should I be concerned about identity theft?
No address / NHS or National Insurance numbers are given out on screen
Those details however can be obtained when reading letters
What if I mess thing up?
No matter what you do or click you can’t alter the records.
You can cancel appointments if you make a mistake
When you order repeat prescriptions, you are given the opportunity to check what you have requested before submitting it and can leave a message with your request
What if I am seeing a doctor and there is no computer in the room?
It can easily happen. If you know you are going to see a doctor then take a print out with you. This could include any of their letters to your GP and any recent test results
What if the doctor I am seeing objects?
Then be polite and apologise
You brought them with you to assist the doctor not to antagonise them
Hilda aged 85 and Jean

Hilda
I am 85 years old. I reside with my daughter and her husband, I suffer with a number of ailments, the most recent of which is gallstones. I have been told by the consultants at the hospital that because of my medical problems I am not really fit to undergo removal by keyhole surgery as there is a risk of me not coming through surgery. I suffer with diabetes, under-active thyroid, diverticular disease, stage 3 chronic kidney disease, angina, loss of hearing, Parkinsons and also osteoarthritis.
I now suffer with insulin dependent diabetes mellitus, having tried to control my condition by both diet and tablet. I have had mixed results using insulin. Some days my readings have been very high and I have also suffered a number of hypos. These seem to happen when one of my other conditions seems to be giving me problems.
My diabetes affects me in a way that I feel very tired all the time and I find that I am very unsteady on my feet and really cannot go unattended. My daughter administers my insulin. The medication for my other problems comes in dossette packs from the pharmacy.
Jean
Hilda lives with my husband and me and we try and look after her to the best of our abilities. This is not the first time we have encountered suffering from diabetes however.
My father, who died at the age of 70, suffered from diabetes for a number of years. Although the doctors recommended him to use insulin, he resisted this for a number of years as he was of the opinion that this was their last resort. During the final years of his life, my father confided in both mum and I that he wished he had started on insulin earlier as it made him feel so much better. However, he died of heart failure in 2001.
For my part, I find the website the surgery has developed has been a great help and has lightened the strain of everyday life by enabling me to book appointments, order repeat prescriptions and to check the results of tests carried out. Also, I can see what recommendations the doctor or nurse have made and the dosage of medications prescribed. I can check these at any time of the day and night if I am unsure of anything and should an emergency doctor have to be called then I cold of course let him have access to all mum’s medical records at the press of a button.
The website makes both of us feel that we are not looking after mum on our own but that we have a network of people we can turn to such as doctors, nurses and support staff.
I would really recommend anyone who is in doubt about the benefits of the surgery website not to worry.
When Dr Hannan first suggested I go to it my first thoughts were “Can anyone get access to my medical records other than me?”
Well no, as long as you keep your password safe then like anything else, it’s personal to you. Also you do not have to be a computer geek to get to the information you require. It’s easy to use and once you are used to it, it will save you time and give you confidence to know you can get to a doctor or medical information at the push of a button.
There is also a wealth of further information on the website and I would urge you to have a go and see the benefit it can make to you and your family.
Hilda & Jean
Received 9th November 2014
Message from Haughton Thornley Medical Centres
Hilda and Jean from Haughton Vale surgery came along to support the Magical Diabetes Event (organised by Louise Brady @louisebrady17 and Susan Mason-Cave @susanmason66) where they presented their views to the audience and encouraged others to join them and work with their clinicians to help feel more in control of their health. Currently over 30% of patients at Haughton Thornley Medical Centres have access to their records and are encouraged to understand their records with the support of all the staff and the practice-based web portal www.htmc.co.uk.
Many older people become frail as they get older and are often reliant on their carers and family to support them. Hilda and Jean have described how they have organised their care having been provided with the “tools” and the information needed to help them. They have also shown how the staff in the practice are supporting them so that they can continue to manage at home away from the practice. Our knowledge is increasing so that how people managed their care before, even 10 years ago, is now changing as new opportunities arise. They are not alone and we are seeing many more patients, families and others asking how to do this too.
A number of practices locally have started offering access to their records too. We are working hard to encourage others to start too. Practices working in partnership with the community to support understanding of healthcare needs and encourage people to adopt more healthier lifestyles is key to regaining the control and for us to support each other. Listen to Eric Evanson, Chair of Donneybrook surgery Patient Participation Group present his views on why this is essential for everybody
We salute all the wonderful people who have come together to share their knowledge and experience so that others may benefit too. There may not be much we can do about the choices we made in the past but there are choices to be made now. Just reading this is a choice you have made and hopefully this will encourage you to move to the next level.
Words and ideas do change the world….one person at a time until suddenly everybody asks “What’s the big deal? We have always done it this way!”.
Dr Hannan
Haughton Thornley Medical Centres
Viewing your blood tests online at Haughton Thornley Medical Centres
On 17th September 2014, Haughton Thornley Patient Participation Group and the practice came together to discuss with patients how they can view their blood tests online and how patients can understand what the test results mean. Please watch the video below to hear what was discussed. We would like to thank Dr Tetlow, consultant clinical scientist at Tameside Hospital Foundation Trust, nurses and patients for helping to make this event a success.
We recommend
- You ask the doctor or nurse why you are having a blood test and what it means
- You can also see what the doctor or nurse has written in the notes when the blood test was organised.
- You can see the comments doctors have written next to the test results
- Please use Lab Tests Online to help you understand what the blood test means and common questions related to the test which is the best source of information on what blood tests mean and how best to understand them
- You can also click on the blue information button next to the test to see generic information of a general nature
- There are other trusted resources on this website to help you understand your condition better. We have done the hard work to find relevant information for you and signpost you to information you can trust rather than just doing a random search which may or may not provide you with good quality information.
- Please remember to ask your doctor or nurse if you do not understand – we are here to help you
Please click on the link below to go to Lab Tests Online and also to download a free app for your IPhone or android device

The Kings Fund blog: Using technology to build a partnership of trust with patients

Amir showed me how patients access their own health records and gain a better understanding of their health care needs. Access and understanding are enabled by the use of apps that provide full online access to the GP electronic health record alongside the practice-based web portal. Patients are also able to book appointments, order repeat prescriptions and send two-way secure messages online.
Two-thirds of the 12,500 people registered with the practice have signed up (after an individual consenting process) for the online service and all the patients I met were aware of the service and were using it. This is a much higher coverage than in the rest of general practice, where the most recent GP patient survey shows awareness of online services offered by GP practices is still relatively low with use of these services considerably lower. The last survey showed only 3.3 per cent of respondents were accessing their medical records online.
Access to records and understanding are the foundations on which Amir, his partners and other colleagues have sought to build a partnership of trust with patients and staff. They are doing so in a practice that was formerly run by Harold Shipman, who achieved notoriety when he was convicted of murdering some of his patients between the 1970s and the 1990s. The commitment to responsible sharing and partnership has helped restore confidence in the care that is provided, and the practice was recently rated outstanding by the Care Quality Commission.
I saw how this works by sitting in on Amir’s morning clinic with his patients. The philosophy I observed was of patients being enabled to take more control of their health and wellbeing, for example, by checking test results, identifying and flagging any errors or omissions, and tracking trends in their care. Later in the day, I tested my observations in a roundtable discussion chaired by Ingrid Brindle who leads the practice’s patient participation group.
One of the benefits for patients is that they can share their records when they come into contact with other services and with family and carers. The latter is valuable for patients who are not confident in using online access themselves. There are particular benefits for patients with long-term conditions who are able to monitor their conditions and use information on their records to adjust their choices.
Reflecting on what I saw and heard, I was reminded of a phrase I heard many years ago on a visit to Kaiser Permanente in California, US. One of its medical leaders, David Sobell, told me that the most important primary care providers are patients themselves; the decisions patients take every day have a bigger impact on their health and care than those made by GPs, nurses and other clinicians. Systems like Kaiser Permanente had been slow to recognise this and Sobell was leading work to promote greater self-care by patients.
The NHS has also been slow to turn the rhetoric of patient engagement and patient empowerment into practice. The experience of Amir Hannan, Ingrid Brindle and their colleagues shows that progress is possible where there is a sustained commitment to develop a partnership of trust with patients. To be sure, the Haughton Thornley Medical Centres have more to do to get all clinicians, patients and the wider health and social care system involved, but their work demonstrates what can be achieved even within the limitations of existing systems and workload pressures.
What I saw was an example of the kind of NHS we need in the future, based on different relationships between patients and clinicians. These relationships have to be seen as meetings of equals in which the expertise of patients is at least as important as the expertise of clinicians and managers. They must acknowledge the responsibilities of patients as well as their rights and the vital contribution of patients in using information and understanding to improve their own health and wellbeing.
Technology can support this transformation, but fundamentally it is about a new deal with the public appropriate for the 21st century. As Derek Wanless warned in 2002, the public must be fully engaged in their care, otherwise the NHS will become unsustainable. The accumulation of many more locally led innovations, such as the one I observed, offers one promising way of heeding his warning and putting patients at the heart of care. I was left puzzled as to why all practices aren’t yet working in this way.
Testimonials from Patients who have got access to their GP electronic health records
Have you ever wondered what the point of getting access to your records is? You can hear about all the potential benefits there might be as well as the challenges. But sometimes, it’s just easier to hear somebody else’s personal story – how it helped them and why it has helped them.
This is a page dedicated to patients at Haughton Thornley Medical Centres describing in their own words what Records Access means for them. Please read their stories and then think about whether you should also consider getting access to your records too.
If you would like to know how to get access to your own records then please click here
If you would like to send your own personal story then please send an email to [email protected] and we would be happy to share it with the world. This is your practice. This is your life. This is your story. In your hands.
Read about G H who at the age of 65 following an emergency admission into hospital requiring the insertion of a cardiac pacemaker, got himself a computer in order to get access to his records. He and his wife learned about how to go online and then found many other useful information which helped him to regain his interest in gardening, change his lifestyle and now feels much better and are enjoying life together. His blood pressure has improved too as a result!
Read about the mother of twins whose son developed blisters and needed urgent care. He had previously needed to go and see a dermatologist to get the correct treatment. Now she simply had to log into her son’s record and share the relevant history, correspondence and medication with the doctor to save time and get the right treatment quickly and easily. Happy parent, happy child and happy clinician.
Read about Mrs S P who describes how her family and friends are very impressed with the service she is enjoying. She is able to book appointments, order repeat prescriptions and access her GP electronic health records has. She has a bad back and has had a scan done showing what discs are involved. She has recently had some blood tests done and instead of booking in to see the doctor or nurse she can….
Read about Mrs G C who at the age of 76 books appointments online, order prescriptions online and last year when she had to go to the hospital…
Read about I H who suffers with White Coat Syndrome which meant her blood pressure was always high whenever she came to the surgery to have her blood pressure checked. She learned about how she could check her own blood pressure at home and then legitimately present an average of her home readings to show that her blood pressure was well-controlled. She learned more about hypertension by looking at the Map of Medicine and then after talking to the doctor, could check in her online medical records that she could check her own blood pressure at home herself and bring the readings along to show the nurse instead of getting worked up about it and worried about her next appointment…
Read about Mrs K M who describes her husband’s health problems including previous heart surgery which means that when he gets chest pains, there is a worry that it might be his heart again. Access to his records means that he does not need to see the doctor immediately or worry if he cannot get in to be seen sooner for non-urgent problems. She also suffers with knee pains but knows that surgery is not an option yet so she has to try to make do as best as she can. She is the main “family health manager” and is able to order prescriptions, book appointments, learn about her own conditions and her husband’s and manage things herself as best as she can. This helps the family to keep going.
Read about Mr AJF, a patient who had already got access to his medial records. But he really saw the benefit when he had a test done and then got a phone call from the receptionist asking for Dr Hannan to speak to him about the results. Normally he would have panicked but now…
Read about Mr JC, a patient with prostate cancer who is able to track his prostate cancer, his regular blood test results and provide them to specialists outside the surgery when they need them.
Read about Mr R and Mrs G F and how they went to the hospital because the husband needed to be seen by a specialist. Following the appointment, he went to see the GP who knew nothing about the consultation at the hospital. The patient was able to check that the letter had not come and was able to take things into his own hands and challenge the hospital to ensure the GP was kept informed.
Read about Mrs P C who does not suffer with any life-threatening problems but has developed a number of eye conditions that could threaten her eye-sight. However she realises to overcome her fear of eye loss, it is important to access reliable, trusted information to help her be kept truly informed…
Read about H N’s wife who went for a pre-operative assessment and was asked her current medication list. Within a few seconds she was able to go online and show her repeat prescriptions and the benefits this accrued including encouraging the healthcare worker to ask for the same service for herself too!
Read about the daughter of one of our Bengali-speaking patients who looks after their parents’ health. When she moved away from the family home, she continued to look after her family’s needs
Read about D D who in March 2017 needed an appointment to see the doctor and was then referred for a Chest Xray. He decided to conduct an “experiment” to see what the experience was like and posted his findings on Facebook for all to see.
Read about I B who has been accessing her records for a long time now, saving her a lot of time and effort by being able to keep an eye on her record and also recognises that this has freed up time for the practice too so that other patients can be seen quicker too…
She also did a presentation in 2011 at an NHS North-West sponsored event for patients and the public on her experience too. Watch her video as she describes to the audience what this means for her and how it helps her get the best from the local healthcare services.
Here is a short video by the late Margaret Rickson aged 84 talking about what Records Access means for her. She was due to present at a conference but was too unwell to come and so produced this video in the hope that others may learn too. You are never too old to learn and do this for yourself but you do need a little help and support from the practice and the clinicians too!
Read how the niece (from Australia) who had Power of Attorney of a patient of Haughton Thornley Medical Centres in a residential home who became terminally ill and how Records Access helped the neice to be kept in touch even though lived on the opposite side of the planet and was able to see what was happening almost in real-time as the record was updated and as her aunt gradually passed away. (Patients now have to apply for Lasting Power of Attorney including Health and Welfare to do this formally and legally).
Electronic Health Records: There are many benefits but what about the risks?
Sarah Blake notes there are benefits but what about the risks ?
Many of us are already using online healthcare facilities. ‘Patient Access’ has been available for some time. I use it myself for convenient repeat prescriptions. The area of digital health technology is growing at a phenomenal rate as it is being incorporated into apps and internet access. Government policy intends that ‘electronic personal health records’ will eventually be accessible to every adult in the UK via the internet and are supporting an NHS app to help create this future vision. This means that patient investigation results, prescriptions, health files and appointment booking facilities will be available for the general population to access from their personal computers and smartphones.
Practices have already started to use a ‘lite’ or ‘full’ version of the online access system and believe that it has brought improvements to the care of their patients. They believe that gaining access to and understanding online medical access is liberating for doctors and empowering for patients and increases patient understanding and involvement in their health care. In essence ‘no decision about me without me.’
Dr Amir Hannan, his patients and practice are huge advocates of online health technology, which enables a Partnership of Trust through Records Access and Understanding. They probably understand the importance of responsible sharing and trust in patient care more than anyone, as it is the same practice that the infamous mass murderer Harold Shipman used to work in. The practice has been a pioneer in electronic health record access and understanding and has enabled over 8,100 patients to use this service (over 65% of his patients). They advocate for a ‘partnership of trust’ between patients, carers and clinicians and think that it is essential to focus on the relationship that a patient or carer has with their GP or nurse who knows them, instead of ad hoc appointments with any GP or nurse. He believes patient care is all about trusting relationships that are developed over time.
‘The doctor/ patient relationship is changing. For generations, it has generally taken the form of an adult/child relationship, but this is shifting. Patients are far more involved in their healthcare. Living longer with chronic long-term conditions means that an approach whereby patients take greater responsibility for their health and healthcare can lead to better outcomes. There are no ‘magic bullet’ solutions but having record access and understanding combined with a ‘partnership of trust’ with the lead clinician can lead to safer, more efficient and productive services. We use an online Records Access and Understanding Safety Checklist questionnaire before signing people up to online services. It includes a safety checklist which helps patients to understand the facility they are signing up to. We have safeguarding policies and procedures in place to help protect vulnerable patients as well and this is part of the comprehensive safety we offer all our patients and staff.’
This seems like a sensible approach to online care and making sure that online care becomes an additional and valuable tool and resource that can be used to enhance patient care rather than a substitution sounds beneficial to many. However, there will still be challenges to face in implementing this technology. Some patients are living in an environment of manipulation, exploitation and coercion from the people who may be closest to them. It has been suggested that under these circumstances having ‘electronic personal health records’ available at home could compromise the healthcare of a substantial number of people.
Approximately one in three people will experience abuse in their lifetime. Those in abusive relationships tend to visit their GP more frequently than the general population as they have more mental and physical health conditions. Their abusive situation is rarely visible to the medical practitioners as it operates under the dynamics of coercive control and could be under the guise of a carer or an attentive partner. Identifying domestic abuse and understanding when someone is really consenting, rather than complying to record access will be a complicated task for any healthcare professional. To make this already complex situation even more tricky is the issue that many people do not realise they are in an abusive relationship, and that the person that they trust has an agenda of undermining and exploiting them.
‘Patient Access’ has been advertised on electronic screens in surgeries as a ‘safe way to share your medical information with family.’ For anyone sat in a waiting room with an abusive partner, a message such as this would make it incredibly difficult to keep personal records private. Perhaps marketing ‘online healthcare’ as a private facility, to only be shared in exceptional circumstances, could help reduce the risk to patients. Well-developed password security may be beneficial. Domestic abuse awareness in practices and an attempt to gain a fully understood and informed consent could also reduce risks. One size does not fit all and having a patient-centred approach will be essential in creating a safer implementation process.
Most people involved in the application of these policies and technological advancements will be trying to manage the delicate balance of safe, efficient and cost-effective healthcare for a diverse range of needs, which will vary across time and locations. For some patients, face-to-face contact with health professionals may literally be a ‘lifeline’ to support. With increasing technological dependency and home prescription deliveries, it’s important to make sure that potentially vulnerable patients do not become further isolated. Making sure that technology does not threaten the ‘safe space’ of confidential and private healthcare appointments is a challenge for the future.
Confused patients – in need of “.com” ?
by Bruce Elliott
Confused patients – in need of ‘.com’?
We have one of the best and most efficient health systems in the world. Having had Type 1 Diabetes since 1970, and a life full of football and fell walking related bumps, strains and breaks I’m so grateful for the NHS. It’s special.
And yet despite this great track record I have to confess that most of my friends and family talk just as much about waits, uncertainty and feeling a bit lost in the health and care system as they do about the wonders of the care that they’re receiving.
When it comes to providing personalised healthcare advice and support I think that ‘Confused’ is one of the most prevalent terms used and ‘.com’ is very rarely seen or offered to my friends or relatives. So I wondered if ‘.com’ can ever help them or provide a solution to the huge demand pressures facing health and care services?
Nearly all my friends have parents in their late 70s, 80s and even a couple in their 90s. In most cases their parents live quite a distance away and few are digitally or ‘.com’ savvy. In the past 6 months alone rather than just sharing the joys of being in our 50s when we meet together, many have been worrying about their parents coping with:
- Not fully understanding what’s been said or diagnosed in GP or Consultant consultations,
- Dementia and the resultant confusion,
- Dates and transport issues for hospital appointments,
- Wondering if District Nurses, Specialist Nurses or Care Assistants really have been notified by their GP or Consultant and if and when they’ll be visiting,
- Understanding, or knowing if plans are in place for hospital discharge,
- Being able to get home assessments undertaken and care plans and packages in place for family members after debilitating strokes, or falls.
Some of the evidence indicates that my friends and relatives, although special, are very much the norm when it comes to understanding and retaining health information.
Studies have indicated that about 50% of information provided by healthcare providers is retained. Another study has painted an even less optimistic picture stating that less than 10% of information is retained. However, evidence seems to show that for most of us between 40 to 80% of what we’re told in a consultation is forgotten immediately.
And it gets worse as the study goes on to show that about half of the information we do think we remember is recalled incorrectly.
Can ‘.com’ provide a solution to improve patient safety, clinical efficiency and reduce confusion? I’m certain that it can at least help, and it has already for me. However, to do this I think that we all need to:
- View it from our own perspective as patients or carers, and then
- Be ACE:
Ask for and Access your medical records online:
As part of my work in the NHS I was lucky enough to meet the members of the Patient Participation Group at Haughton-Thornley Medical Practice in Hyde. Many of the people that I met had been former patients of the infamous Harold Shipman. One of the GPs who came to Hyde after the terrible crimes of Harold Shipman were uncovered was Dr Amir Hannan. Amir believes in the importance of building a ‘Partnership of Trust’ with patients and actively encourages them to build up a better understanding of their condition and how best to manage it. Accessing their GP medical record is an essential part of this and over 59% of the patients at Haughton-Thornley now do so, including 82% of my fellow Type 1 Diabetics.
Nationally though still only 5.2 per cent of GP patients report that they are aware that their practice offers them the ability to access their records online and only 0.9 per cent of them have used this feature (NHS England and Ipsos MORI 2016).
Having access to my medical records has been of enormous benefit to me from understanding diagnoses, seeing that referral letters have been sent, viewing test results to check how good my control has been, and in ensuring that prescriptions which I’ve ordered online are ready for me to pick up at my chosen Pharmacy.
Ideally your GP should recommend access to you, particularly if you have a Long Term Condition. However, in practice you’re more likely to have to ask for access yourself.
Contribute your own health information and knowledge to your Care Team:
I test my blood glucose levels 7 or 8 times a day. I can add them directly to apps which then show clear trends. I can upload and input details of my activity levels, the food that I eat, my sleep patterns and even track how my stress levels caused by my love of Sunderland Football Club impact on my control.
I have to manage and understand my condition 365 days a year. I’d be very happy to share my results with my Diabetologist, Diabetes Specialist Nurse and GP. I’d be over the moon if I could share it with researchers too to help find potential triggers and cures. I’d be ecstatic if I could share it with Medical and Nursing students to help build their understanding of Type 1 Diabetes in their training. However, few ever ask for it and only one has ever suggested how I could best share it with them.
Now I could do this via my own Personal Health Record (PHR), such as Patients Know Best which would also link to all my other Health Records too from my hospital care as well as my GP. I could send it to my Care Team once a year and flag any concerns I have. You never know it could save me having to take time off work and let another patient who really wants help and advice take my place.
There are national commitments in place within existing Health and Care policies and plans in England to try and encourage us all to collect and contribute this sort of information. These include the ‘Five Year Forward View’ and ‘Personalised Health and Care 2020’ where commitments are given, for example to:
- having an accredited Health Apps Library in place by 2017,
- being able to view information from all health and social care interactions by April 2018
- being able to add comments and preferences to records by April 2018
Ideally members of your Care Team should recommend suitable PHRs to you. But at the moment there’s little knowledge of their use, even in good practices like my own, and so why not use one of the many PHRs yourself and help to contribute to their learning and education as well as to your Health and Care record.
Educate and Enthuse others:
If you’re a ‘Confused’ patient and feel that after reading this that ‘.com’ may help you then help is at hand. The Patient Information Forum has just released a new Education Guide to PHRs, which will link you to a whole series of links, case studies and other practical resources.
The new guide aims to assist, educate and enthuse Patients, Clinicians and, in fact, all Health and Care staff and remove the confusion.
Going back to my own friends many of them also represent one of the most important groups of people that we need to enthuse, Carers. If you’re a ‘Confused’ Carer and your parent, partner or loved one is losing the ability to care for themselves you can help them, if they wish, to apply to give you consent to access their records, order repeat prescriptions and book appointments by proxy . Or if you have lasting power of attorney you can request access yourself on their behalf.
And so I believe that there is a way for all of us to reduce the time, worry and confusion you might have caring for you and your family by:
- booking your appointments and prescriptions online
- reading about your diagnoses, referrals, appointments and care plans online
- sharing your own test results and fitness levels with the people who care for you
As a Type 1 Diabetic, Husband, Dad, Son, Son-in-law, Brother, Uncle and NHS Manager I would love that to be the norm. In fact if we use ‘.com’ more it would be ‘ACE’.
The views expressed in this article are personal. If the ideas have enthused you and you’d like further guidance please let me know and I’ll try and help or provide introductions to many of the wonderful people who sparked my interest in Patient Online Access back in 2007 and have kept it burning ever since. Bruce Elliott 14/10/16 Contact: [email protected] or Tweet @bruceelliottuk
Footnote:
After sharing this blog one of my friends, whose wonderful Mam had a severe stroke earlier this year and is now in a Nursing Home, shared some sad reflections on his experiences. As well as trying to arrange the care that his Mam needed he also had to ensure that support for his 90 year old Dad was in place to help him to continue to live at home independently.
‘I definitely endorse what you are saying. The lack of communication between NHS, local authorities, Social Services and other agencies causes problems throughout the system. It can take weeks and months to get relevant information by which time a situation may be beyond rectification. Much of the communication is by telephone, often there is no email or messaging option. So you may have a series of missed calls, then speak with someone who has no access to the relevant records.
In many businesses we see the successful use of email, messaging and electronic audit trail systems so that all concerned can view the status of a process and a full record of what has been said and done. A similar system for healthcare would make a massive difference. All concerned would be informed on arrangements required, for example follow-up treatment being booked.’
So many of these challenges could be overcome by the ways that I have outlined in my blog.
British Medical Journal blog: Demand online access to your medical records, says Richard Smith
by Richard Smith in the BMJ, February 18, 2009
I’ve just emailed my GP asking her to give me online access to my medical records. It was quite a palaver as I couldn’t find her email address, or the email address of the practice after searching on Google, and the practice doesn’t seem to have a website. Eventually I had to ring.
Why have I never done this before? I spend half my life online. Most of my work is done online. I shop, manage my finances, and do my taxes online. My web footprint is huge. So why have I never asked for access to the most intimate details about me that are kept on a computer about a mile from here? Well, it never occurred to me — just as it hasn’t occurred to virtually everybody in Britain and the entire audience at a Cambridge seminar I attended last night full of the digerati. It’s culture, stupid.
The audience was urged to contact their GPs and ask for online access to their records by Dr Amir Hannan, the GP successor to Harold Shipman in Hyde, Greater Manchester. His challenge was to rebuild trust in a practice where it had been totally destroyed. The day before he started there was a sit down protest in the surgery, and Shipman’s relatives came and took away all the computers.
Dr Hannan saw giving patients access to their records as an important step in building what he calls a “partnership of trust.” Some 600 (3%) of his patients now have access to their records online, and he believes that moving to “real time digital medicine” is transforming health care.
Patients can access all the information about them, make appointments, order repeat prescriptions, and access lots of information and decision support tools. The result is increased health literacy, better concordance, improved accuracy in the records, and a trusting adult to adult relationship that itself improves health. Those patients who have online access to their records can’t understand why everybody doesn’t do it.
With the EMIS system, which is used by 60% of GPs, it is easy, and cost free, to give patients access to their records. But only 40 practices in the country have done it so far—we are very much at the beginning of this revolution. Dr Hannan, a huge enthusiast, says that he has had no problems from the change, but interestingly most of the questions from the audience were about the downside of the change (security, confidentiality, etc) not the considerable upside.
The meeting also heard from Dr Mohammad Al-Ubaydli, a doctor and founder of Patients Know Best, who has studies personal health records at UCL’s Centre for Health Informatics and Multiprofessional Education.
A personal health record is one that the patient rather than the doctor controls, and this is surely where we must be headed. There is published evidence showing that personal health records can produce many benefits, are particularly valuable for patients with chronic conditions, and improve compliance and care. Interaction is better than simply access, and “coauthorship” between patients and doctors creates accuracy and concordance.
You can access both presentations at http://wiki.patientsknowbest.com/Patients_Know_Best/Lectures/2009.02.17_Using_Personal_Health_Records_in_the_NHS, and I urge you right now to ask your GP for online access to you records. Both you and she will benefit.
Competing interest: Richard Smith is an unpaid member of the board of Patients Know Best and a true believer that the web can ultimately transform health care as it is transforming so much else.
BBC Radio Manchester interview of Dr Hannan

Dr Hannan got interviewed by Sam Walker from BBC Radio Manchester on 9th December 2013 at the Brooke Surgery in Hyde. They had spent the morning in the surgery interviewing different people to show what the surgery is like and some of the challenges faced by staff, patients and the clinicians as they try to deliver high quality services under very challenging circumstances.
Dr Hannan was asked a variety of questions including why patients would want access to their records, will they understand what they read or will they become confused by it, would they even be allowed to look at their records and how could it help them and their loved ones.
Haughton Thornley Medical Centres has been enabling patients to access their records since 2006 and has accrued a great deal of expertise along the way on how to do it, what works and how it should be done. It has also learned a lot about some of the challenges that we are facing and how to meet those challenges, Listen to the radio item below and see what you think. We have also provided links to specific issues that were raised in the radio item for you to learn more.
BBC Radio Manchester Interview of Richard Fitton
Health 2.0 Manchester “live” consultation with patient and with Dr Hannan
BBC News
Web records prove hit with patients by Jane Dreaper
Royal College of General Practice’s Guidance for health professionals
The limits of health data aggregation – why our health records don’t tell our whole stories
by Katie McKurdy January 9th, 2019
I like to keep up with news about health innovation, technology, and startups. I find it interesting, and as a designer working in healthcare I need to stay informed.
In browsing healthcare technology news from various outlets, I’ve noticed that a lot of it is about health data — how it’s siloed (sorry to use that word); how and why it should be aggregated; how it should easily flow between systems; how patients should own and control it.
These are all true and good things. But I’ve noticed that there’s a ‘holy grail’ mentality when it comes to interoperability and aggregation; a sense that if we could only bring all the data together in one place, we’d finally have a complete picture of a person and be able to diagnose and treat them more effectively.
In my recent work helping patients assemble and communicate about their health histories with Pictal Health, I’ve learned about what information they consider important and spent a lot of time working to visually represent that information. Their stories are filled with life events, theories, feelings, and nuance only they can provide. Here is a sample patient timeline:
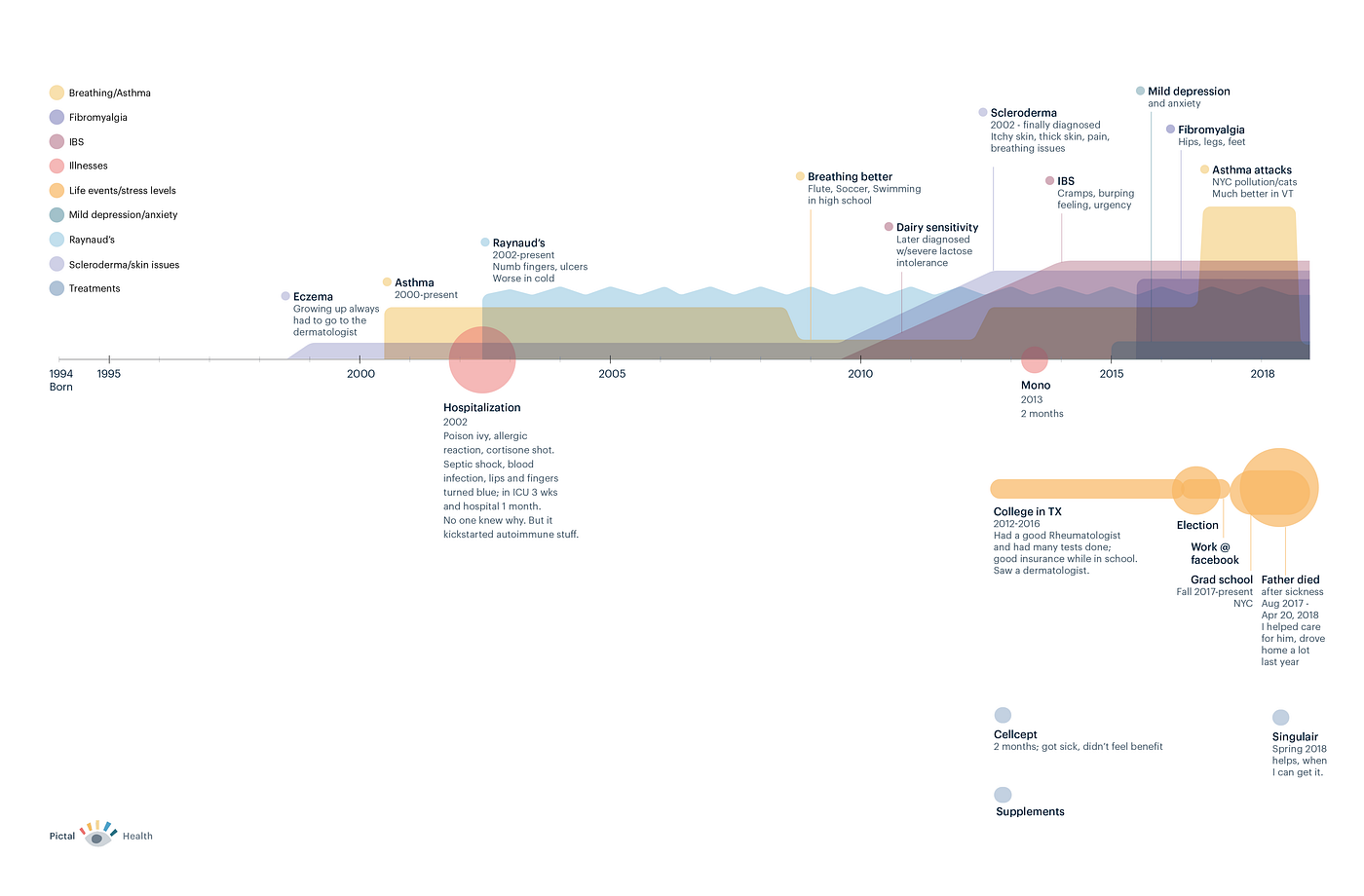
When I compare these visual, holistic stories to the health records I’ve encountered, I can say with confidence that data aggregation alone cannot produce a person’s whole health story. Here are a few reasons why.
1. Medical records have rampant errors.
An estimated 70 percent of medical records have errors. These may be egregious, like Abby Norman’s record incorrectly stating she has 8 sisters (she has none), or they might be small, like a name misspelling.
My own medical record has a ‘problem’ (diagnosis) that is no longer active, and honestly it’s an embarrassing thing that I’d like to have archived off of my active problem list. Every time I go to the doctor and have an ‘after-visit summary’ printed, it shows this private issue on it. I’ve tried to get it updated a few times, and I haven’t had any luck. Unfortunately, it’s not uncommon for patients like me to have difficulty fixing medical record mistakes.
Sometimes our medical records misrepresent us because of their inherent limitations, rather than outright errors. I recently worked with a woman who accessed her medical records from a large California hospital system. She gave me a complete list of all of her conditions, medications, allergies, etc; her medication list in particular had over 50 items on it, many of which she did not recognize or was sure she never actually took. Our medical records are good at showing when a medication was prescribed, but bad at indicating whether we took the medication or for what duration of time. In order to put together an accurate picture, we had to groom through her data manually and determine which medications she took, and fix the dates associated with them.
So, while our medical records are important repositories of our history, they’re often filled with medications we never took, diagnoses entered by accident, and conditions we no longer have. Bringing all of this information together is helpful and a good first step, but we also need a process of sifting through it to fix the errors, omissions and inconsistencies; patients should be at the center of this process.
2. Medical records have a ton of data; not all of it is relevant to your story.
The sheer amount of information collected about us in our records, especially if we’ve had multi-day hospital stays, becomes overwhelming. Lab tests, doctor’s notes, procedure results; our records become a swirl of medical and scientific facts, billing codes, doctors’ thoughts and opinions about what’s happening with us, and more. This information is vital and life-saving in many cases.
But it can be paralyzing to try to make sense out of the huge amount of data about a given patient, and medical record systems do not make it easy to understand the big picture. Providers are forced to click through many different sections of the chart and read through a lot of old notes to try to get a sense of a person’s story. Multiple healthcare providers have expressed a variation of the following statement to me:
“It is incredibly painful to find a patient’s story in their chart.”
There are surely insights to be gained through natural language processing and machine learning, but these findings will nonetheless always be constrained by the limited nature what’s actually included in our records. Which leads me to my next points.
3. Aggregation is mostly about digital data, but unless we are very young, a lot of our story is still on paper (or in our heads).

I was born in 1978. When I was growing up in the quaint hamlet of Cadillac, MI, my doctors took handwritten notes or typed them up. I do have some photocopies of paper records from a neurologist I saw in my teens and twenties, but at this point, my earlier childhood records are very likely no longer around; according to the Miller Canfield lawfirm, “Under the Michigan Public Health Code, medical records must be retained for a minimum period of seven years following the last date of service provided to a patient.” So if my mom and dad didn’t request print-outs of all my records when I was young, those records are now probably gone.
But a lot of interesting things happened when I was younger. I had allergies throughout childhood, stomach issues as a 10-year old, swollen joints and overuse of antibiotics as a tween, and other precursors to autoimmune and rheumatological conditions. No doctor would be able to find those details in my current digital medical record, but in telling my life story I wouldn’t want these factors to be left out.
4. Large swaths of our human existence are not captured in our medical records.
- Our symptom and bodily experiences are not well-represented in our records. Medical staff ask us how much pain we feel on a 1–10 scale, but this doesn’t capture important details about the quality of our pain, what it looks and feels like, how it travels, and more. The pain scale is a blunt tool, and a one-dimensional view of how we are doing at any given moment; it does not tell much of a story.
- When we look into our deep past, we can often remember times when our symptoms were worse or better; these stand out as symptom milestones of a sort. In October of 1997, I got double vision for the first time and had to have a series of plasmapheresis treatments. I no longer have any records from that time except some spotty doctor’s notes, but I clearly remember what happened, almost to the week. Sitting in the back of a large lecture hall, I recall squinting at my professor and being unable to focus correctly on him unless I closed one eye. In November 1997, I trekked across frosty campus sidewalks at dawn on my way get my plasma exchanged (3 days per week) at the University of Michigan medical center. I also started taking prednisone for the first time, and I was embarrassed to see my face swelling up (a common side effect) even while I was relieved that my symptoms were subsiding. These events aren’t easily available in my current medical record, but they are foundational to my personal journey, and they are easy for me to recall — often with a cinematic level of detail.
- Many parts of ‘life’ that have a direct impact on our wellbeing, such as stress, traumatic events, social support, exercise, and diet are not well-captured in our medical records. Consider how a death in the family, a divorce, being laid off, or moving across the country might impact your health; these are some of the most important events of our lives, but our doctors can’t easily locate them in our records.
- Stress, in particular, is something we talk about all the time; we read self-help books and articles, we meditate, we exercise, we medicate, all in an effort to reduce our stress. But stress, as a concept, is not well-represented in a structured way in our medical records.
- Related to stress, mental health (not just mental illness) is often a gaping hole in our medical records. If I see a private therapist because I need emotional support with some aspect of my life, that fact is not likely to make it into my medical record. But since our mental and physical health are so intertwined, it would be helpful for my doctors to know if I’m going through a rough patch mentally.
Conclusions
Go ahead, put all my health data together into one big pile. It’s an important first step, but it’s still going to be missing about half of my story.
We need to work with patients to groom and refine the data, discard the junk, and add layers of meaning. We need to enable people to tell their whole health stories, not just via the structured data that exists in our health records, but to represent the multiple facets of their mental, physical and social health.
Because the fact is, important clues lie in our stories that could help us get the correct diagnosis and treatment.
I care about this partly because I’m working on a way for patients to tell their health stories visually, with Pictal Health; but it’s also the right thing to do.
Cancer Mum: So why do patients and carers want Health Records?
by Cancer Mum 19th april 2019
So finally, here it is, news from the front line in my first @Cancer Mum blog. For those who follow me on Twitter you will already know my Tweets about patient record access are passionate, angry, frustrated, impatient, relentless and some have said simplistic. There are many commentators on the subject and it is a topic that attracts comments from around the world. It’s hard to explain the real message in a few words on social media but there is a message to be told and it must be heard.
So why is medical record access so important to people like me, why do we fight so vociferously and challenge the system?
Our story started in 2005 when our healthy fourteen-year-old teenager was suddenly diagnosed with a rare brain tumour. It was large, growing from the pituitary fossa backwards compressing his brain stem and descending down into his cervical canal. Surgery to debunk the tumour left us with a teenager with multiple disabilities due to a brain stem stroke and a poor prognosis tumour. Over the years an unbelievable number of care providers have touched us on the worst journey a family could imagine. The last fifteen years have been a roller coaster and secondary care has been a constant feature in our son’s life creating a significant amount of information. As my son’s main carer I have managed all his medical care from the first year when it became clear that the provision was split across many providers and only our family knew the overall picture in a complicated jigsaw of care.
My interest in collating an accessible online health account began as I approached a milestone birthday. Like most parents who care for a child whose life is compromised by ill health or disability I started to look to the future. As parents we will not always be here to manage his care with our vast knowledge of events. So, there were questions.
- Who would take over the complicated management?
- Who knew all the details accumulated over the years?
- How complete was his medical record?
- Does he have a medical record?
- Where is his medical record?
- Could we create a fully shareable online health account that would ensure safe care in the future?
So, the journey of discovery began. My starting point was application for full access to my son’s GP record. My concern at this point was to ensure that all the paper information our family had in many files was available in the GP record. The application for full online record access met with outright rejection and it was there my fight started. A statement was issued by the practice stating that it was not mandatory to share free text or historical letters and this would not change until they were required to do so.
Almost a year later, during a visit to the practice by a RCGP Digital Champion on our behalf, it became clear that there was no electronic GP record. I had been fighting for information that didn’t exist. I had been unaware that my son’s electronic records had not followed him, unaware paper records were stored off site, unaware that no significant documents had been scanned into the new electronic record, unaware that a clerk had created an incorrect summary list, unaware that access to any historical letters and consultation text would continue to be refused. Transparency and partnership working were not on the agenda. After this visit a large amount of documentation from the paper record was scanned onto the new electronic record at the request of the visiting GP.
Advertisements
about:blank
REPORT THIS ADPRIVACY
Further investigation revealed that transfer of all GP records has been patchy for a number of years. There is a short transfer window for the GP2GP transfer process and if the patient record is not called within the timeframe the file is locked and cannot be retrieved at a later date.
This is an important point as the failure to transfer GP electronic records when patients relocate has a significant effect on information flow and creates silos of information in the chain.
Further investigation showed an unexpected reality, my son’s data set is summarised in the flow chart below
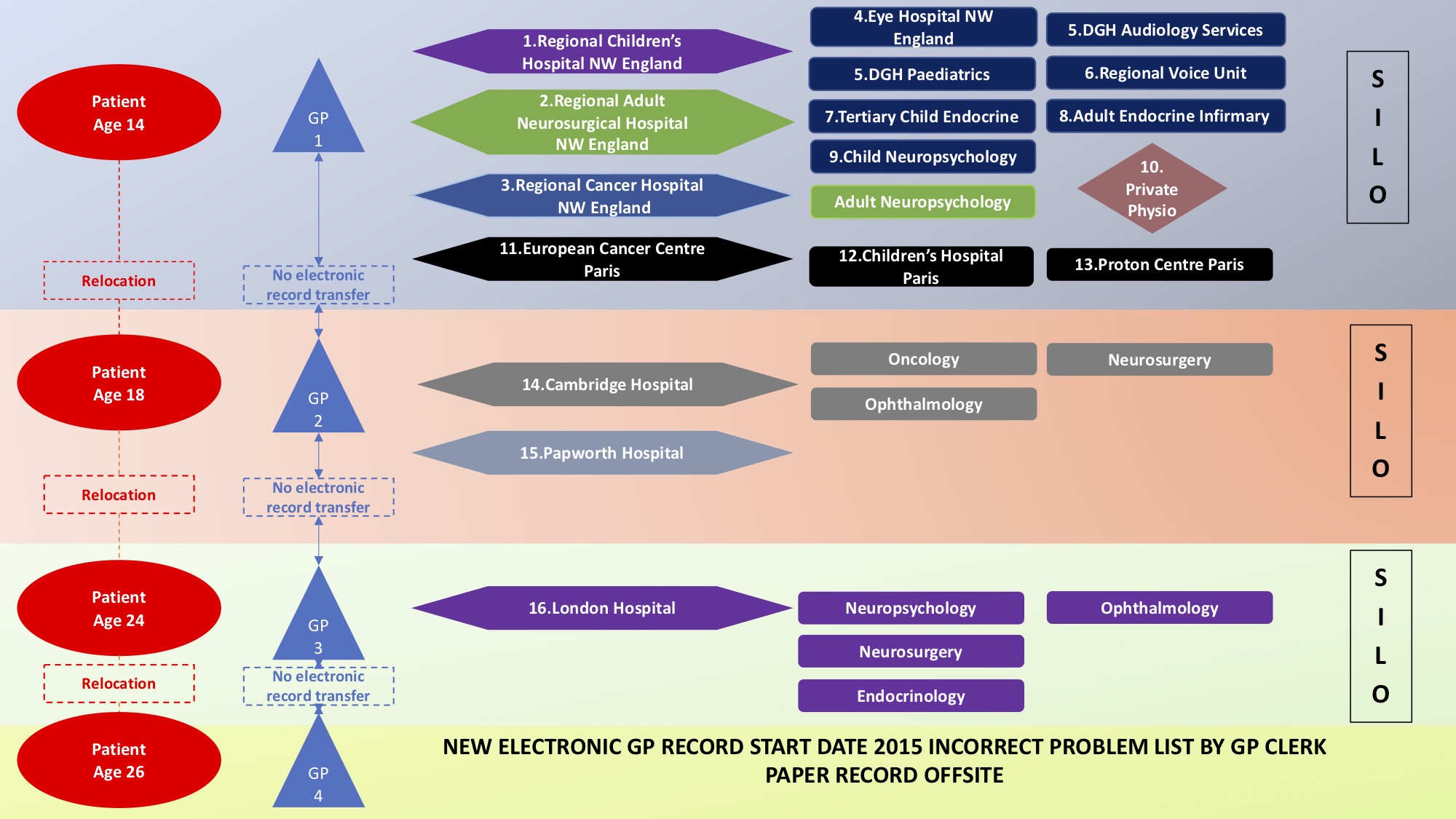
The following table illustrates the multiple conditions that needed continuing care across the years. The lack of information at each new point of care required repeated explanations of a long and complex history by the family. Inevitably with the vast number of health interactions over a fourteen year period our memory of the details of separate events became increasing blurred.
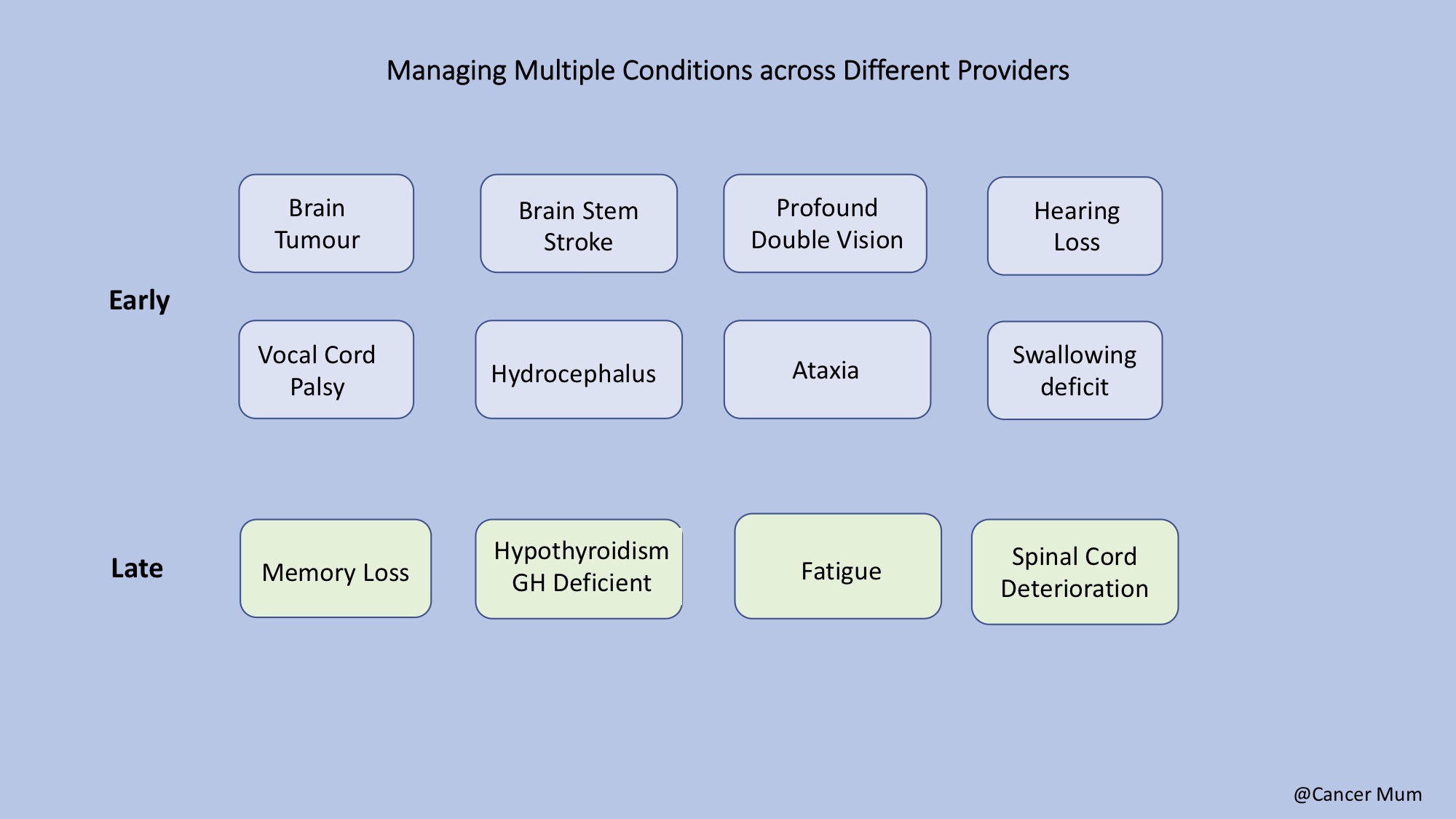
Our son’s health record in numbers.
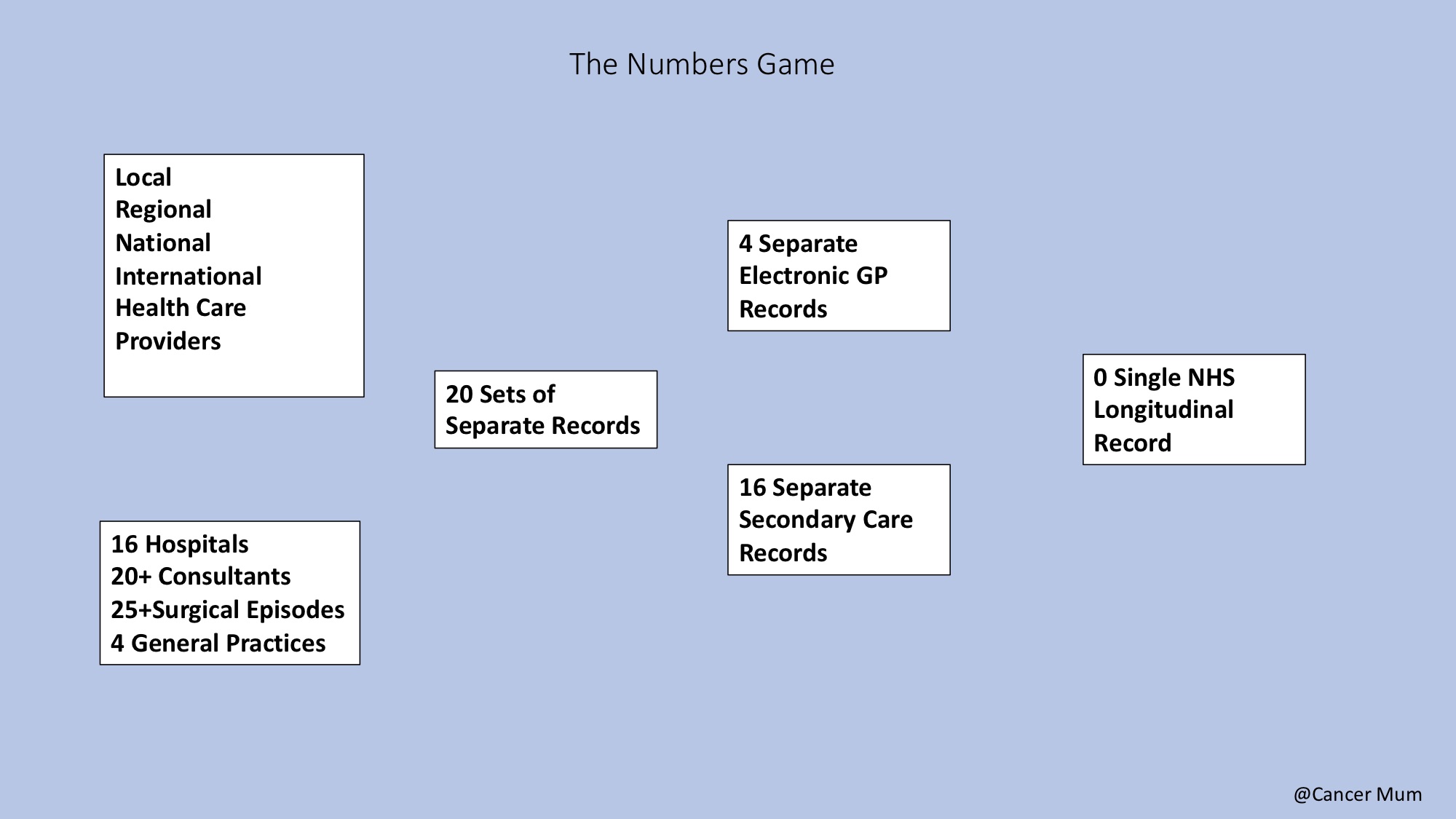
At the end of December 2017 following the failure of the RCGP Digital Champion to secure full access to the free text and historical letters in my son’s online GP record I decided to issue notice to the practice that I would take formal action using the Equalities Act 2010. I requested ‘reasonable adjustments’ to be made to mitigate for hearing impairment and severe memory deficit. The Practice agreed to facilitate full record access after a partner meeting. My son remains the only patient in a 40,000 group practice list to have this access.
After a period of six weeks in May last our son became ill quite suddenly. There was clear indication that his neurological status had changed. He was admitted in severe pain to a major neurological centre through the Accident and Emergency Department. He was seen by the neurosurgical team who had not met him before and there was no medical record of the complex surgery and conditions in the flow charts above. The impaired neurological picture indicated a cervical spinal cord issue. Words cannot adequately explain our terror as parents at this point.
We tried to answer as many questions as we could but the stress made it difficult. We were unable to name the French Hospitals or remember the details of the previous cervical spine laminectomies. Then we remembered the new online GP account and accessed it through an App on a phone. To our shock there were hundreds of document and consultation entries but they were not indexed and useless. I have talked about this here
Our son went on to have urgent brain and spinal surgery and he has since recovered well. It is a situation I would not wish on any family. We learnt from our experience and now we have a fully indexed longitudinal patient record created using the Evergreen Life App. I have transferred all relevant documents over the last fourteen years and the account is fully shareable by all member of our family.
Stop, Look and Listen
Advertisements
about:blank
REPORT THIS ADPRIVACY
Despite continued promises of access to all our health information by successive politicians and the talk of new gateways to our health information linking primary, secondary and social care, to people like us it seems as far away as ever. We hear about the Empowering the Person initiative, projects to improve data flows, data standards and all those new Apps but citizens like us are still as helpless as ever standing next to that stretcher in A/E without the very basic information to save our loved one’s life in a crisis.
The announcement today of the new London SCRa mobile which allows ambulance staff to access records for front line care is good news. So much good work is coming from NHS Digital but how effective will this be if the Summary Care Record information is extracted from inaccurate and incomplete patient records? My son’s allergies have been missed in the paper muddle. Is the risk of sudden intracranial bleed noted? Do we need to stop and look at the basics?
Is anyone listening? Despite years of campaigning for full GP record access by clinicians and patients alike the new five-year GMS contract only mandated full patient access to prospective records. The choice to release historical free data remains the choice of individual GP practices. What use is that to patients with complex histories? How can they manage their care? That door is closed for the next five years.
I have recently become involved with the procurement evaluation stage of our Local Health and Care Record. Patients are not considered stakeholders. There has been no citizen engagement prior to specification. The specification has been put together by the professional users with no thought to what we might need or want. The patient portal is parked in the future. Access to a full longitudinal NHS record is another five years away in reality. Another door closed for five years.
These developments have caused our family great concern and frustration. We just want to keep our son safe.
We are being let down.
The sound of doors slamming shut is deafening.
Getting the most from a hospital appointment
How Haughton Thornley Medical Centres engages patients and staff!
Shared Medical Records benefit Patients and Doctors
Haughton Thornley Medical Centres in Hyde, Greater Manchester has been enabling patients and carers to have
full access to their electronic health records and gain a better understanding of their healthcare needs since
All patients are encouraged to sign up so that they can see what the GP or practice nurse has written in
the notes and see results of tests and letters back from the hospital as soon as they arrive in the surgery.
Responsibly sharing the record with patients and carers allows them to feel more in control of their healthcare
and be better prepared when they visit the hospital with up-to-date information on their smartphone / tablet or
PC to share with others. The practice-based web portal www.htmc.co.uk supports patients and staff enabling
each to learn and share. See https://tinyurl.com/HTMCHospitalAppointment
Click here to read more
